NHP 2017
Source: https://www.nhp.gov.in/
1. Introduction
The National Health Policy of 1983 and the National Health Policy of 2002 have served well in guiding the approach for the health sector in the Five-Year Plans. Now 14 years after the last health policy, the context has changed in four major ways. First, the health priorities are changing. Although maternal and child mortality have rapidly declined, there is growing burden on account of non-communicable diseases and some infectious diseases. The second important change is the emergence of a robust health care industry estimated to be growing at double digit. The third change is the growing incidences of catastrophic expenditure due to health care costs, which are presently estimated to be one of the major contributors to poverty. Fourth, a rising economic growth enables enhanced fiscal capacity. Therefore, a new health policy responsive to these contextual changes is required.
The primary aim of the National Health Policy, 2017, is to inform, clarify, strengthen and prioritize the role of the Government in shaping health systems in all its dimensions- investments in health, organization of healthcare services, prevention of diseases and promotion of good health through cross sectoral actions, access to technologies, developing human resources, encouraging medical pluralism, building knowledge base, developing better financial protection strategies, strengthening regulation and health assurance.
NHP 2017 builds on the progress made since the last NHP 2002. The developments have been captured in the document “Backdrop to National Health Policy 2017- Situation Analyses”, Ministry of Health & Family Welfare, Government of India.
2. Goal, Principles and Objectives
2.1 Goal
The policy envisages as its goal the attainment of the highest possible level of health and well-being for all at all ages, through a preventive and promotive health care orientation in all developmental policies, and universal access to good quality health care services without anyone having to face financial hardship as a consequence. This would be achieved through increasing access, improving quality and lowering the cost of healthcare delivery.
The policy recognizes the pivotal importance of Sustainable Development Goals (SDGs). An indicative list of time bound quantitative goals aligned to ongoing national efforts as well as the global strategic directions is detailed at the end of this section.
2.2 Key Policy Principles
I. Professionalism, Integrity and Ethics: The health policy commits itself to the highest professional standards, integrity and ethics to be maintained in the entire system of health care delivery in the country, supported by a credible, transparent and responsible regulatory environment.
II. Equity: Reducing inequity would mean affirmative action to reach the poorest. It would mean minimizing disparity on account of gender, poverty, caste, disability, other forms of social exclusion and geographical barriers. It would imply greater investments and financial protection for the poor who suffer the largest burden of disease.
III. Affordability: As costs of care increases, affordability, as distinct from equity, requires emphasis. Catastrophic household health care expenditures defined as health expenditure exceeding 10% of its total monthly consumption expenditure or 40% of its monthly non-food consumption expenditure, are unacceptable.
IV. Universality: Prevention of exclusions on social, economic or on grounds of current health status. In this backdrop, systems and services are envisaged to be designed to cater to the entire population- including special groups.
V. Patient Centered & Quality of Care: Gender sensitive, effective, safe, and convenient healthcare services to be provided with dignity and confidentiality. There is need to evolve and disseminate standards and guidelines for all levels of facilities and a system to ensure that the quality of healthcare is not compromised.
VI. Accountability: Financial and performance accountability, transparency in decision making, and elimination of corruption in health care systems, both in public and private.
VII. Inclusive Partnerships: A multi stakeholder approach with partnership & participation of all non-health ministries and communities. This approach would include partnerships with academic institutions, not for profit agencies, and health care industry as well.
VIII. Pluralism: Patients who so choose and when appropriate, would have access to AYUSH care providers based on documented and validated local, home and community based practices. These systems, inter alia, would also have Government support in research and supervision to develop and enrich their contribution to meeting the national health goals and objectives through integrative practices.
IX. Decentralization: Decentralization of decision making to a level as is consistent with practical considerations and institutional capacity. Community participation in health planning processes, to be promoted side by side.
X. Dynamism and Adaptiveness: constantly improving dynamic organization of health care based on new knowledge and evidence with learning from the communities and from national and international knowledge partners is designed.
2.3 Objectives
Improve health status through concerted policy action in all sectors and expand preventive, promotive, curative, palliative and rehabilitative services provided through the public health sector with focus on quality.
2.3.1 Progressively achieve Universal Health Coverage
A. Assuring availability of free, comprehensive primary health care services, for all aspects of reproductive, maternal, child and adolescent health and for the most prevalent communicable, non-communicable and occupational diseases in the population. The Policy also envisages optimum use of existing manpower and infrastructure as available in the health sector and advocates collaboration with non -government sector on pro-bono basis for delivery of health care services linked to a health card to enable every family to have access to a doctor of their choice from amongst those volunteering their services.
B. Ensuring improved access and affordability, of quality secondary and tertiary care services through a combination of public hospitals and well measured strategic purchasing of services in health care deficit areas, from private care providers, especially the not-for profit providers
C. Achieving a significant reduction in out of pocket expenditure due to health care costs and achieving reduction in proportion of households experiencing catastrophic health expenditures and consequent impoverishment.
2.3.2 Reinforcing trust in Public Health Care System: Strengthening the trust of the common man in public health care system by making it predictable, efficient, patient centric, affordable and effective, with a comprehensive package of services and products that meet immediate health care needs of most people.
2.3.3 Align the growth of private health care sector with public health goals: Influence the operation and growth of the private health care sector and medical technologies to ensure alignment with public health goals. Enable private sector contribution to making health care systems more effective, efficient, rational, safe, affordable and ethical. Strategic purchasing by the Government to fill critical gaps in public health facilities would create a demand for private health care sector, in alignment with the public health goals.
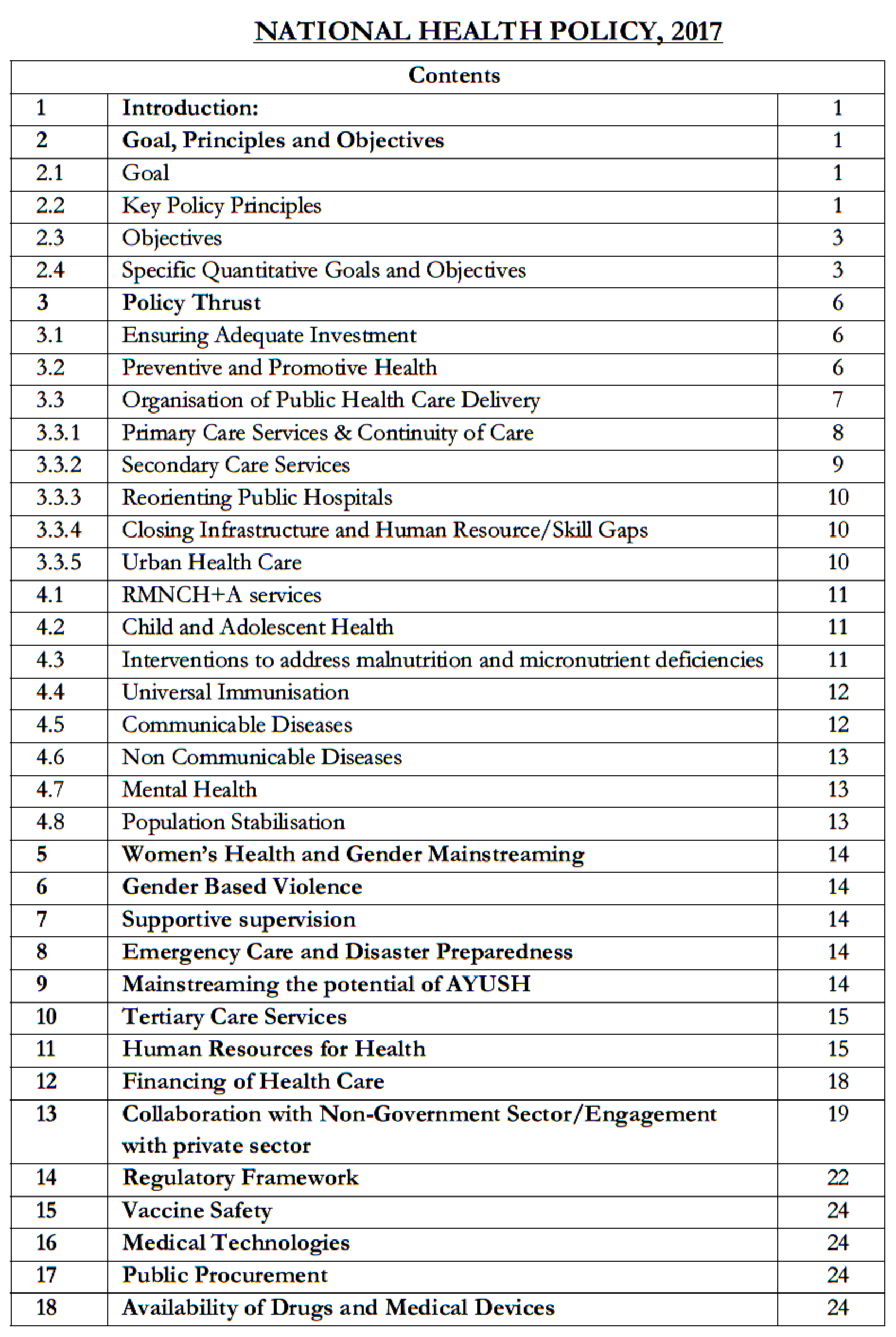
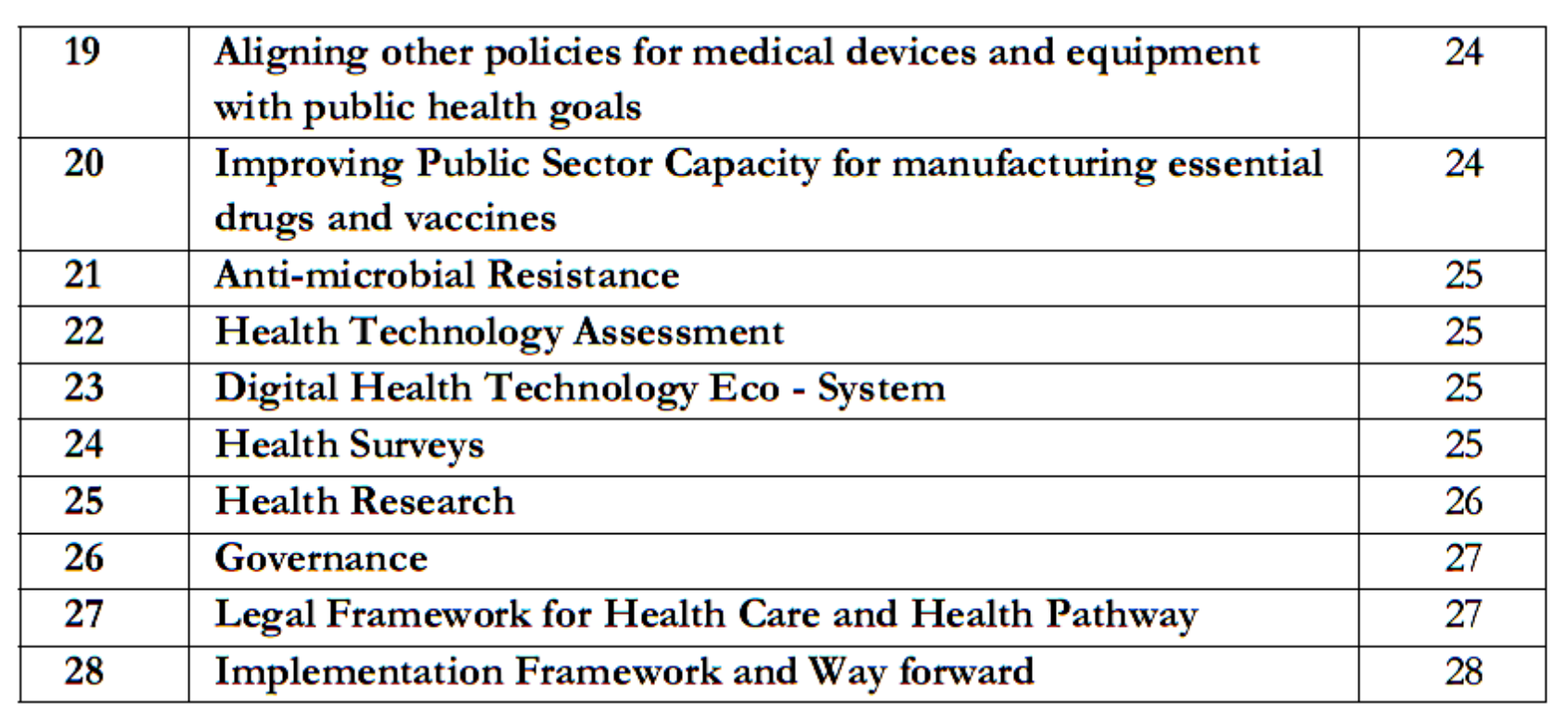
2.4 Specific Quantitative Goals and Objectives:
The indicative, quantitative goals and objectives are outlined under three broad components viz. (a) health status and programme impact, (b) health systems performance and (c) health system strengthening. These goals and objectives are aligned to achieve sustainable development in health sector in keeping with the policy thrust.
2.4.1 Health Status and Programme Impact
- Life Expectancy and healthy life
- Increase Life Expectancy at birth from 67.5 to 70 by 2025.
- Establish regular tracking of Disability Adjusted Life Years (DALY) Index as a measure of burden of disease and its trends by major categories by 2022.
- Reduction of TFR to 2.1 at national and sub-national level by 2025.
2.4.1.2 Mortality by Age and/ or cause
- Reduce Under Five Mortality to 23 by 2025 and MMR from current levels to 100 by 2020.
- Reduce infant mortality rate to 28 by 2019.
- Reduce neo-natal mortality to 16 and still birth rate to “single digit” by 2025.
2.4.1.3 Reduction of disease prevalence/ incidence
- Achieve global target of 2020 which is also termed as target of 90:90:90, for HIV/AIDS i. e,- 90% of all people living with HIV know their HIV status, – 90% of all people diagnosed with HIV infection receive sustained antiretroviral therapy and 90% of all people receiving antiretroviral therapy will have viral suppression.
- Achieve and maintain elimination status of Leprosy by 2018, Kala-Azar by 2017 and Lymphatic Filariasis in endemic pockets by 2017.
- To achieve and maintain a cure rate of >85% in new sputum positive patients for TB and reduce incidence of new cases, to reach elimination status by 2025.
- To reduce the prevalence of blindness to 0.25/ 1000 by 2025 and disease burden by one third from current levels.
- To reduce premature mortality from cardiovascular diseases, cancer, diabetes or chronic respiratory diseases by 25% by 2025.
2.4.2 Health Systems Performance
2.4.2.1 Coverage of Health Services
- Increase utilization of public health facilities by 50% from current levels by 2025.
- Antenatal care coverage to be sustained above 90% and skilled attendance at birth above 90% by 2025.
- More than 90% of the newborn are fully immunized by one year of age by 2025.
- Meet need of family planning above 90% at national and sub national level by 2025.
- 80% of known hypertensive and diabetic individuals at household level maintain “controlled disease status‟ by 2025.
2.4.2.2 Cross Sectoral goals related to health
- Relative reduction in prevalence of current tobacco use by 15% by 2020 and 30% by 2025.
- Reduction of 40% in prevalence of stunting of under-five children by 2025.
- Access to safe water and sanitation to all by 2020 (Swachh Bharat Mission).
- Reduction of occupational injury by half from current levels of 334 per lakh agricultural workers by 2020.
- National/ State level tracking of selected health behaviour.
2.4.3 Health Systems strengthening
2.4.3.1 Health finance
- Increase health expenditure by Government as a percentage of GDP from the existing 1.15% to 2.5 % by 2025.
- Increase State sector health spending to > 8% of their budget by 2020.
- Decrease in proportion of households facing catastrophic health expenditure from the current levels by 25%, by 2025.
2.4.3.2 Health Infrastructure and Human Resource
- Ensure availability of paramedics and doctors as per Indian Public Health Standard (IPHS) norm in high priority districts by 2020.
- Increase community health volunteers to population ratio as per IPHS norm, in high priority districts by 2025.
- Establish primary and secondary care facility as per norms in high priority districts (population as well as time to reach norms) by 2025.
2.4.3.3 Health Management Information
- Ensure district-level electronic database of information on health system components by 2020.
- Strengthen the health surveillance system and establish registries for diseases of public health importance by 2020.
- Establish federated integrated health information architecture, Health Information Exchanges and National Health Information Network by 2025.
3. Policy Thrust
3.1 Ensuring Adequate Investment The policy proposes a potentially achievable target of raising public health expenditure to 2.5% of the GDP in a time bound manner. It envisages that the resource allocation to States will be linked with State development indicators, absorptive capacity and financial indicators. The States would be incentivized for incremental State resources for public health expenditure. General taxation will remain the predominant means for financing care. The Government could consider imposing taxes on specific commodities- such as the taxes on tobacco, alcohol and foods having negative impact on health, taxes on extractive industries and pollution cess. Funds available under Corporate Social Responsibility would also be leveraged for well-focused programmes aiming to address health goals.
3.2 Preventive and Promotive Health The policy articulates to institutionalize inter-sectoral coordination at national and sub-national levels to optimize health outcomes, through constitution of bodies that have representation from relevant non-health ministries. This is in line with the emergent international “Health in All” approach as complement to Health for All. The policy prerequisite is for an empowered public health cadre to address social determinants of health effectively, by enforcing regulatory provisions.
The policy identifies coordinated action on seven priority areas for improving the environment for health:
o The Swachh Bharat Abhiyan
o Balanced, healthy diets and regular exercises.
o Addressing tobacco, alcohol and substance abuse
o Yatri Suraksha – preventing deaths due to rail and road traffic accidents
o Nirbhaya Nari –action against gender violence
o Reduced stress and improved safety in the work place
o Reducing indoor and outdoor air pollution
The policy also articulates the need for the development of strategies and institutional mechanisms in each of these seven areas, to create Swasth Nagrik Abhiyan –a social movement for health. It recommends setting indicators, their targets as also mechanisms for achievement in each of these areas.
The policy recognizes and builds upon preventive and promotive care as an under-recognized reality that has a two-way continuity with curative care, provided by health agencies at same or at higher levels. The policy recommends an expansion of scope of interventions to include early detection and response to early childhood development delays and disability, adolescent and sexual health education, behavior change with respect to tobacco and alcohol use, screening, counseling for primary prevention and secondary prevention from common chronic illness –both communicable and non-communicable diseases. Additionally the policy focus is on extending coverage as also quality of the existing package of services. Policy recognizes the need to frame and adhere to health screening guidelines across age groups. Zoonotic diseases like rabies need to be addressed through concerted and coordinated action, at the national front and through strengthening of the National Rabies Control Programme.
The policy lays greater emphasis on investment and action in school health- by incorporating health education as part of the curriculum, promoting hygiene and safe health practices within the school environs and by acting as a site of primary health care. Promotion of healthy living and prevention strategies from AYUSH systems and Yoga at the work-place, in the schools and in the community would also be an important form of health promotion that has a special appeal and acceptability in the Indian context.
Recognizing the risks arising from physical, chemical, and other workplace hazards, the policy advocates for providing greater focus on occupational health. Work-sites and institutions would be encouraged and monitored to ensure safe health practices and accident prevention, besides providing preventive and promotive healthcare services.
ASHA will also be supported by other frontline workers like health workers (male/female) to undertake primary prevention for non-communicable diseases. They would also provide community or home based palliative care and mental health services through health promotion activities. These workers would get support from local self-government and the Village Health Sanitation and Nutrition Committee (VHSNC).
In order to build community support and offer good healthcare to the vulnerable sections of the society like the marginalised, the socially excluded, the poor, the old and the disabled, the policy recommends strengthening the VHSNCs and its equivalent in the urban areas.
„Health Impact Assessment‟ of existing and emerging policies, of key non-health departments that directly or indirectly impact health would be taken up.
3.3 Organization of Public Health Care Delivery: The policy proposes seven key policy shifts in organizing health care services
o In primary care – from selective care to assured comprehensive care with linkages to referral hospitals
o In secondary and tertiary care – from an input oriented to an output based strategic purchasing
o In public hospitals – from user fees & cost recovery to assured free drugs, diagnostic and emergency services to all
o In infrastructure and human resource development – from normative approach to targeted approach to reach under-serviced areas
o In urban health – from token interventions to on-scale assured interventions, to organize Primary Health Care delivery and referral support for urban poor. Collaboration with other sectors to address wider determinants of urban health is advocated.
o In National Health Programmes – integration with health systems for programme effectiveness and in turn contributing to strengthening of health systems for efficiency.
o In AYUSH services – from stand-alone to a three dimensional mainstreaming
Free primary care provision by the public sector, supplemented by strategic purchase of secondary care hospitalization and tertiary care services from both public and from non-government sector to fill critical gaps would be the main strategy of assuring healthcare services. The policy envisages strategic purchase of secondary and tertiary care services as a short term measure. Strategic purchasing refers to the Government acting as a single payer. The order of preference for strategic purchase would be public sector hospitals followed by not-for profit private sector and then commercial private sector in underserved areas, based on availability of services of acceptable and defined quality criteria. In the long run, the policy envisages to have fully equipped and functional public sector hospitals in these areas to meet secondary and tertiary health care needs of population, especially the poorest and marginalized. Public facilities would remain the focal point in the healthcare delivery system and services in the public health facilities would be expanded from current levels. The policy recognizes the special health needs of tribal and socially vulnerable population groups and recommends situation specific measures in provisioning and delivery of services. The policy advocates enhanced outreach of public healthcare through Mobile Medical Units (MMUs), etc. Tribal population in the country is over 100 million (Census 2011), and hence deserves special attention keeping in mind their geographical and infrastructural challenges. Keeping in view the high cost involved in provisioning and managing orphan diseases, the policy encourages active engagement with non-government sector for addressing the situation. In order to provide access and financial protection at secondary and tertiary care levels, the policy proposes free drugs, free diagnostics and free emergency care services in all public hospitals. To address the growing challenges of urban health, the policy advocates scaling up National Urban Health Mission (NUHM) to cover the entire urban population within the next five years with sustained financing.
For effectively handling medical disasters and health security, the policy recommends that the public healthcare system retain a certain excess capacity in terms of health infrastructure, human resources, and technology which can be mobilized in times of crisis.
In order to leverage the pluralistic health care legacy, the policy recommends mainstreaming the different health systems. This would involve increasing the validation, evidence and research of the different health care systems as a part of the common pool of knowledge. It would also involve providing access and informed choice to the patients, providing an enabling environment for practice of different systems of medicine, an enabling regulatory framework and encouraging cross referrals across these systems.
3.3.1 Primary Care Services and Continuity of Care:
This policy denotes important change from very selective to comprehensive primary health care package which includes geriatric health care, palliative care and rehabilitative care services. The facilities which start providing the larger package of comprehensive primary health care will be called Health and Wellness Centers‟. Primary care must be assured. To make this a reality, every family would have a health card that links them to primary care facility and be eligible for a defined package of services anywhere in the country. The policy recommends that health centres be established on geographical norms apart from population norms. To provide comprehensive care, the policy recommends a matching human resources development strategy, effective logistics support system and referral backup. This would also necessitate upgradation of the existing sub-centres and reorienting PHCs to provide comprehensive set of preventive, promotive, curative and rehabilitative services. It would entail providing access to assured AYUSH healthcare services, as well as support documentation and validation of local home and community based practices. The policy also advocates for research and validation of tribal medicines. Leveraging the potential of digital health for two way systemic linkages between the various levels of care viz., primary, secondary and tertiary, would ensure continuity of care. The policy advocates that the public health system would put in place a gatekeeping mechanism at primary level in a phased manner, accompanied by an effective feedback and follow-up mechanism.
3.3.2 Secondary Care Services:
The policy aspires to provide at the district level most of the secondary care which is currently provided at a medical college hospital. Basic secondary care services, such as caesarian section and neonatal care would be made available at the least at sub-divisional level in a cluster of few blocks. To achieve this, policy therefore aims:
o To have at least two beds per thousand population distributed in such a way that it is accessible within golden hour rule. This implies an efficient emergency transport system. The policy also aims that ten categories of what are currently specialist skills be available within the district. Additionally four or at least five of these specialist skill categories be available at sub-district levels. This may be achieved by strengthening the district hospital and a well-chosen, well located set of sub-district hospitals.
o Resource allocation that is responsive to quantity, diversity and quality of caseloads provided.
o Purchasing care after due diligence from non-Government hospitals as a short term strategy till public systems are strengthened.
Policy proposes a responsive and strong regulatory framework to guide purchasing of care from non-government sector so that challenges of quality of care, cost escalations and impediments to equity are addressed effectively.
In order to develop the secondary care sector, comprehensive facility development and obligations with regard to human resources, especially specialists needs, are to be prioritized. To this end the policy recommends a scheme to develop human resources and specialist skills.
Access to blood and blood safety has been a major concern in district healthcare services. This policy affirms in expanding the network of blood banks across the country to ensure improved access to safe blood.
3.3.3 Re-Orienting Public Hospitals:
Public hospitals have to be viewed as part of tax financed single payer health care system, where the care is pre-paid and cost efficient. This outlook implies that quality of care would be imperative and the public hospitals and facilities would undergo periodic measurements and certification of level of quality. The policy endorses that the public hospitals would provide universal access to a progressively wide array of free drugs and diagnostics with suitable leeway to the States to suit their context. The policy seeks to eliminate the risks of inappropriate treatment by maintaining adequate standards of diagnosis and treatment. Policy recognizes the need for an information system with comprehensive data on availability and utilization of services not only in public hospitals but also in non-government sector hospitals. State public health systems should be able to provide all emergency health services other than services covered under national health programmes.
3.3.4 Closing Infrastructure and Human Resources/Skill Gaps:
The policy duly acknowledges the roadmap of the 12th Five Year Plan for managing human resources for health. The policy initiatives aim for measurable improvements in quality of care. Districts and blocks which have wider gaps for development of infrastructure and deployment of additional human resources would receive focus. Financing for additional infrastructure or human resources would be based on needs of outpatient and inpatient attendance and utilization of key services in a measurable manner.
3.3.5 Urban Health Care:
National health policy prioritizes addressing the primary health care needs of the urban population with special focus on poor populations living in listed and unlisted slums, other vulnerable populations such as homeless, rag-pickers, street children, rickshaw pullers, construction workers, sex workers and temporary migrants. Policy would also prioritize the utilization of AYUSH personnel in urban health care. Given the large presence of private sector in urban areas, policy recommends exploring the possibilities of developing sustainable models of partnership with for profit and not for profit sector for urban health care delivery. An important focus area of the urban health policy will be achieving convergence among the wider determinants of health – air pollution, better solid waste management, water quality, occupational safety, road safety, housing, vector control, and reduction of violence and urban stress. These dimensions are also important components of smart cities. Healthcare needs of the people living in the peri urban areas would also be addressed under the NUHM. Further, Non-Communicable Diseases (NCDs) like hyper tension, diabetes which are predominant in the urban areas would be addressed under NUHM, through planned early detection. Better secondary prevention would also be an integral part of the urban health strategy. Improved health seeking behavior, influenced through capacity building of the community based organizations & establishment of an appropriate referral mechanism, would also be important components of this strategy.
4. National Health Programmes
4.1 RMNCH+A services: Maternal and child survival is a mirror that reflects the entire spectrum of social development. This policy aspires to elicit developmental action of all sectors to support Maternal and Child survival. The policy strongly recommends strengthening of general health systems to prevent and manage maternal complications, to ensure continuity of care and emergency services for maternal health. In order to comprehensively address factors affecting maternal and child survival, the policy seeks to address the social determinants through developmental action in all sectors.
4.2 Child and Adolescent Health: The policy endorses the national consensus on accelerated achievement of neonatal mortality targets and „single digit‟ stillbirth rates through improved home based and facility based management of sick newborns. District hospitals must ensure screening and treatment of growth related problems, birth defects, genetic diseases and provide palliative care for children. The policy affirms commitment to pre-emptive care (aimed at pre-empting the occurrence of diseases) to achieve optimum levels of child and adolescent health. The policy envisages school health programmes as a major focus area as also health and hygiene being made a part of the school curriculum. The policy gives special emphasis to the health challenges of adolescents and long term potential of investing in their health care. The scope of Reproductive and Sexual Health should be expanded to address issues like inadequate calorie intake, nutrition status and psychological problems interalia linked to misuse of technology, etc.
4.3 Interventions to Address Malnutrition and Micronutrient Deficiencies: Malnutrition, especially micronutrient deficiencies, restricts survival, growth and development of children. It contributes to morbidity and mortality in vulnerable population, resulting in substantial diminution in productive capacity in adulthood and consequent reduction in the nation‟s economic growth and well-being. Recognising this, the policy declares that micronutrient deficiencies would be addressed through a well-planned strategy on micronutrient interventions. Focus would be on reducing micronutrient malnourishment and augmenting initiatives like micro nutrient supplementation, food fortification, screening for anemia and public awareness. A systematic approach to address heterogeneity in micronutrient adequacy across regions in the country with focus on the more vulnerable sections of the population, is needed. Hence, screening for multiple micronutrient deficiencies is advocated. During the critical period of pregnancy, lactation, early childhood, adolescence and old age, the consequences of deficiencies are particularly severe and many are irreversible. While dietary diversification remains the most desirable way forward, supplementation and fortification require to be considered as short and medium term solutions to fill nutrient gaps. The present efforts of Iron Folic Acid(IFA) supplementation, calcium supplementation during pregnancy, iodized salt, Zinc and Oral Rehydration Salts/Solution(ORS), Vitamin A supplementation, needs to be intensified and increased. Sustained efforts are to be made to ensure outreach to every beneficiary, which in turn necessitates that intensive monitoring mechanisms are put in place. The policy advocates developing a strong evidence base, of the burden of collective micronutrient deficiencies, which should be correlated with disease burden and in particular for understanding the etiology of anemia. Policy recommends exploring fortified food and micronutrient sprinkles for addressing deficiencies through Anganwadi centers and schools. Recognising the complementary role of various nutrition-sensitive interventions from different platforms, the policy calls for synergy of inputs from departments like Women and Child Development, Education, WASH, Agriculture and Food and Civil Supplies. Policy envisages that the MoHFW would take on the role of convener to monitor and ensure effective integration of both nutrition-sensitive and nutrition-specific interventions for coordinated optimal results.
4.4 Universal Immunization: Priority would be to further improve immunization coverage with quality and safety, improve vaccine security as per National Vaccine Policy 2011 and introduction of newer vaccines based on epidemiological considerations. The focus will be to build upon the success of Mission Indradhanush and strengthen it.
4.5 Communicable Diseases: The policy recognizes the interrelationship between communicable disease control programmes and public health system strengthening. For Integrated Disease Surveillance Programme, the policy advocates the need for districts to respond to the communicable disease priorities of their locality. This could be through network of well-equipped laboratories backed by tertiary care centers and enhanced public health capacity to collect, analyze and respond to the disease outbreaks.
4.5.1 Control of Tuberculosis: The policy acknowledges HIV and TB co infection and increased incidence of drug resistant tuberculosis as key challenges in control of Tuberculosis. The policy calls for more active case detection, with a greater involvement of private sector supplemented by preventive and promotive action in the workplace and in living conditions. Access to free drugs would need to be complemented by affirmative action to ensure that the treatment is carried out, dropouts reduced and transmission of resistant strains are contained.
4.5.2 Control of HIV/AIDS: While the current emphasis on prevention continues, the policy recommends focused interventions on the high risk communities (MSM, Transgender, FSW, etc.) and prioritized geographies. There is a need to support care and treatment for people living with HIV/AIDS through inclusion of 1st, 2nd and 3rd line antiretroviral(ARV), Hep-C and other costly drugs into the essential medical list.
4.5.3 Leprosy Elimination: To carry out Leprosy elimination the proportion of grade-2 cases amongst new cases will become the measure of community awareness and health systems capacity, keeping in mind the global goal of reduction of grade 2 disability to less than 1 per million by 2020. Accordingly, the policy envisages proactive measures targeted towards elimination of leprosy from India by 2018.
4.5.4 Vector Borne Disease Control: The policy recognizes the challenge of drug resistance in Malaria, which should be dealt with by changing treatment regimens with logistics support as appropriate. New National Programme for prevention and control of Japanese Encephalitis (JE)/Acute Encephalitis Syndrome (AES) should be accelerated with strong component of inter-sectoral collaboration. The policy recognizes the interrelationship between communicable disease control programmes and public health system strengthening. Every one of these programmes requires a robust public health system as their core delivery strategy. At the same time, these programmes also lead to strengthening of healthcare systems.
4.6 Non-Communicable Diseases: The policy recognizes the need to halt and reverse the growing incidence of chronic diseases. The policy recommends to set-up a National Institute of Chronic Diseases including Trauma, to generate evidence for adopting cost effective approaches and to showcase best practices. This policy will support an integrated approach where screening for the most prevalent NCDs with secondary prevention would make a significant impact on reduction of morbidity and preventable mortality. This would be incorporated into the comprehensive primary health care network with linkages to specialist consultations and follow up at the primary level. Emphasis on medication and access for select chronic illness on a „round the year‟ basis would be ensured. Screening for oral, breast and cervical cancer and for Chronic Obstructive Pulmonary Disease (COPD) will be focused in addition to hypertension and diabetes. The policy focus is also on research. It emphasizes developing protocol for mainstreaming AYUSH as an integrated medical care. This has a huge potential for effective prevention and therapy, that is safe and cost-effective. Further the policy commits itself to support programmes for prevention of blindness, deafness, oral health, endemic diseases like fluorosis and sickle cell anaemia/thalassemia,etc. The National Health Policy commits itself to culturally appropriate community centered solutions to meet the health needs of the ageing community in addition to compliance with constitutional obligations as per the Maintenance and Welfare of Parents and Senior Citizens Act, 2007. The policy recognizes the growing need for palliative and rehabilitative care for all geriatric illnesses and advocates the continuity of care across all levels. The policy recognizes the critical need of meeting the growing demand of tissue and organ transplant in the country and encourages widespread public awareness to promote voluntary donations.
4.7 Mental Health: This policy will take into consideration the provisions of the National Mental Health Policy 2014 with simultaneous action on the following fronts:
o Increase creation of specialists through public financing and develop special rules to give preference to those willing to work in public systems.
o Create network of community members to provide psycho-social support to strengthen mental health services at primary level facilities and
o Leverage digital technology in a context where access to qualified psychiatrists is difficult.
4.8 Population Stabilization: The National Health Policy recognises that improved access, education and empowerment would be the basis of successful population stabilization. The policy imperative is to move away from camp based services with all its attendant problems of quality, safety and dignity of women, to a situation where these services are available on any day of the week or at least on a fixed day. Other policy imperatives are to increase the proportion of male sterilization from less than 5% currently, to at least 30% and if possible much higher.
5. Women’s Health & Gender Mainstreaming:
There will be enhanced provisions for reproductive morbidities and health needs of women beyond the reproductive age group (40+) This would be in addition to package of services covered in the previous paragraphs.
6. Gender based violence (GBV):
Women‟s access to healthcare needs to be strengthened by making public hospitals more women friendly and ensuring that the staff have orientation to gender –sensitivity issues. This policy notes with concern the serious and wide ranging consequences of GBV and recommends that the health care to the survivors/ victims need to be provided free and with dignity in the public and private sector.
7. Supportive Supervision:
For supportive supervision in more vulnerable districts with inadequate capacity, the policy will support innovative measures such as use of digital tools and HR strategies like using nurse trainers to support field workers.
8. Emergency Care and Disaster Preparedness:
Better response to disasters, both natural and manmade, requires a dispersed and effective capacity for emergency management. It requires an army of community members trained as first responder for accidents and disasters. It also requires regular strengthening of their capacities in close collaboration with the local self-government and community based organisations. The policy supports development of earthquake and cyclone resistant health infrastructure in vulnerable geographies. It also supports development of mass casualty management protocols for CHC and higher facilities and emergency response protocols at all levels. To respond to disasters and emergencies, the public healthcare system needs to be adequately skilled and equipped at defined levels, so as to respond effectively during emergencies. The policy envisages creation of a unified emergency response system, linked to a dedicated universal access number, with network of emergency care that has an assured provision of life support ambulances, trauma management centers–
o one per 30 lakh population in urban areas and
o one for every 10 lakh population in rural areas
9. Mainstreaming the Potential of AYUSH:
For persons who so choose, this policy ensures access to AYUSH remedies through co-location in public facilities. Yoga would be introduced much more widely in school and work places as part of promotion of good health as adopted in National AYUSH Mission (NAM). The policy recognizes the need to standardize and validate Ayurvedic medicines and establish a robust and effective quality control mechanism for AUSH drugs. Policy recognizes the need to nurture AYUSH system of medicine, through development of infrastructural facilities of teaching institutions, improving quality control of drugs, capacity building of institutions and professionals. In addition, it recognizes the need for building research and public health skills for preventive and promotive healthcare. Linking AYUSH systems with ASHAs and VHSNCs would be an important plank of this policy. The National Health Policy would continue mainstreaming of AYUSH with general health system but with the addition of a mandatory bridge course that gives competencies to mid-level care provider with respect to allopathic remedies. The policy further supports the integration of AYUSH systems at the level of knowledge systems, by validating processes of health care promotion and cure. The policy recognizes the need for integrated courses for Indian System of Medicine, Modern Science and Ayurgenomics. It puts focus on sensitizing practitioners of each system to the strengths of the others. Further the development of sustainable livelihood systems through involving local communities and establishing forward and backward market linkages in processing of medicinal plants will also be supported by this policy. The policy seeks to strengthen steps for farming of herbal plants. Developing mechanisms for certification of „prior knowledge‟ of traditional community health care providers and engaging them in the conservation and generation of the raw materials required, as well as creating opportunities for enhancing their skills are part of this policy.
10. Tertiary care Services:
The policy affirms that the tertiary care services are best organized along lines of regional, zonal and apex referral centers. It recommends that the Government should set up new Medical Colleges, Nursing Institutions and AIIMS in the country following this broad principle. Regional disparities in distribution of these institutions must be addressed. The policy supports periodic review and standardization of fee structure and quality of clinical training in the private sector medical colleges. The policy enunciates the core principle of societal obligation on the part of private institutions to be followed. This would include:
o Operationalization of mechanisms for referral from public health system to charitable hospitals.
o Ensuring that deserving patients can be admitted on designated free / subsidized beds.
The policy proposes to consider forms of resource generation, where corporate hospitals and medical tourism earnings are through a high degree of associated hospitality arrangements and on account of certain procedures and services, as a form of resource mobilization towards the health sector. The policy recommends establishing National Healthcare Standards Organization and to develop evidence based standard guidelines of care applicable both to public and private sector. The policy shows the way forward in developing partnership with non-government sector through empaneling the socially motivated and committed tertiary care centers into the Government efforts to close the specialist gap.
To expand public provisioning of tertiary services, the Government would additionally purchase select tertiary care services from empaneled non-government sector hospitals to assist the poor. Coverage in terms of population and services will expand gradually. The policy recognizes development of evidence based standard guidelines of care, applicable both to public and private sector as essential.
11. Human Resources for Health:
There is a need to align decisions regarding judicious growth of professional and technical educational institutions in the health sector, better financing of professional and technical education, defining professional boundaries and skill sets, reshaping the pedagogy of professional and technical education, revisiting entry policies into educational institutions, ensuring quality of education and regulating the system to generate the right mix of skills at the right place. This policy recommends that medical and para-medical education be integrated with the service delivery system, so that the students learn in the real environment and not just in the confines of the medical school. The key principle around the policy on human resources for health is that, workforce performance of the system would be best when we have the most appropriate person, in terms of both skills and motivation, for the right job in the right place, working within the right professional and incentive environment.
11.1 Medical Education: The policy recommends strengthening existing medical colleges and converting district hospitals to new medical colleges to increase number of doctors and specialists, in States with large human resource deficit. The policy recognizes the need to increase the number of post graduate seats. The policy supports expanding the number of AIIMS like centers for continuous flow of faculty for medical colleges, biomedical and clinical research. National Knowledge Network shall be used for Tele-education, Tele-CME, Tele-consultations and access to digital library. A common entrance exam is advocated on the pattern of NEET for UG entrance at All India level; a common national-level Licentiate/exit exam for all medical and nursing graduates; a regular renewal at periodic intervals with Continuing Medical Education (CME) credits accrued, are important recommendations. This policy recommends that the current pattern of MCQ (Multiple Choice Question) based entrance test for post graduates medical courses- that drive students away from practical learning- should be reviewed. The policy recognizes the need to revise the under graduate and post graduate medical curriculum keeping in view the changing needs, technology and the newer emerging disease trends. Keeping in view, the rapid expansion of medical colleges in public and private sector there is an urgent need to review existing institutional mechanisms to regulate and ensure quality of training and education being imparted. The policy recommends that the discussion on recreating a regulatory structure for health professional education be revisited to address the emerging needs and challenges.
11.2 Attracting and Retaining Doctors in Remote Areas: Policy proposes financial and non-financial incentives, creating medical colleges in rural areas; preference to students from under-serviced areas, realigning pedagogy and curriculum to suit rural health needs, mandatory rural postings, etc. Measures of compulsion- through mandatory rotational postings dovetailed with clear and transparent career progression guidelines are valuable strategies. A constant effort, therefore, needs to be made to increase the capacity of the public health systems to absorb and retain the manpower. The total sanctioned posts of doctors in the public sector should increase to ensure availability of doctors corresponding to the accepted norms. Exact package of policy measures would vary from State to State and would change over time.
11.3 Specialist Attraction and Retention: Proposed policy measures include – recognition of educational options linked with National Board of Examination & College of Physicians and Surgeons, creation of specialist cadre with suitable pay scale, up-gradation of short term training to medical officers to provide basic specialist services at the block and district level, performance linked payments and popularise MD (Doctor of Medicine) course in Family Medicine or General Practice. The policy recommends that the National Board of Examinations should expand the post graduate training up to the district level. The policy recommends creation of a large number of distance and continuing education options for general practitioners in both the private and the public sectors, which would upgrade their skills to manage the large majority of cases at local level, thus avoiding unnecessary referrals.
11.4 Mid-Level Service Providers: For expansion of primary care from selective care to comprehensive care, complementary human resource strategy is the development of a cadre of mid-level care providers. This can be done through appropriate courses like a B.Sc. in community health and/or through competency-based bridge courses and short courses. These bridge courses could admit graduates from different clinical and paramedical backgrounds like AYUSH doctors, B.Sc. Nurses, Pharmacists, GNMs, etc and equip them with skills to provide services at the sub-centre and other peripheral levels. Locale based selection, a special curriculum of training close to the place where they live and work, conditional licensing, enabling legal framework and a positive practice environment will ensure that this new cadre is preferentially available where they are needed most, i.e. in the under-served areas.
11.5 Nursing Education: The policy recognises the need to improve regulation and quality management of nursing education. Other measures suggested are – establishing cadres like Nurse Practitioners and Public Health Nurses to increase their availability in most needed areas. Developing specialized nursing training courses and curriculum (critical care, cardio-thoracic vascular care, neurological care, trauma care, palliative care and care of terminally ill), establishing nursing school in every large district or cluster of districts of about 20 to 30 lakh population and establishing Centers of Excellence for Nursing and Allied Health Sciences in each State. States which have adequate nursing institutions have flexibility to explore a gradual shift to three year nurses even at the sub-centre level to support the implementation of the comprehensive primary health care agenda.
11.6 ASHA: This policy supports certification programme for ASHAs for their preferential selection into ANM, nursing and paramedical courses. While most ASHAs will remain mainly voluntary and remunerated for time spent, those who obtain qualifications for career opportunities could be given more regular terms of engagement. Policy also supports enabling engagements with NGOs to serve as support and training institutions for ASHAs and to serve as learning laboratories on future roles of community health workers. The policy recommends revival and strengthening of Multipurpose Male Health Worker cadre, in order to effectively manage the emerging infectious and non-communicable diseases at community level. Adding a second Community Health Worker would be based on geographic considerations, disease burdens, and time required for multiple tasks to be performed by ASHA/ Community Health Worker.
11.7 Paramedical Skills: Training courses and curriculum for super specialty paramedical care (perfusionists, physiotherapists, occupational therapists, radiological technicians, audiologists, MRI technicians, etc.) would be developed. The policy recognises the role played by physiotheraphists, occupational and allied health professionals keeping in view the demographic and disease transition the country is faced with and also recognises the need to address their shortfall. Planned expansion of allied technical skills- radiographers, laboratory technicians, physiotherapists, pharmacists, audiologists, optometrists, occupational therapists with local employment opportunities, is a key policy direction. The policy would allow for multi-skilling with different skill sets so that when posted in more peripheral hospitals there is more efficient use of human resources.
11.8 Public Health Management Cadre: The policy proposes creation of Public Health Management Cadre in all States based on public health or related disciplines, as an entry criteria. The policy also advocates an appropriate career structure and recruitment policy to attract young and talented multi-disciplinary professionals. Medical & health professionals would form a major part of this, but professionals coming in from diverse backgrounds such as sociology, economics, anthropology, nursing, hospital management, communications, etc. who have since undergone public health management training would also be considered. States could decide to locate these public health managers, with medical and non-medical qualifications, into same or different cadre streams belonging to Directorates of health. Further, the policy recognizes the need to continuously nurture certain specialized skills like entomology, housekeeping, bio-medical waste management, bio medical engineering communication skills, management of call centres and even ambulance services.
11.9 Human Resource Governance and leadership development: The policy recognizes that human resource management is critical to health system strengthening and healthcare delivery and therefore the policy supports measures aimed at continuing medical and nursing education and on the job support to providers, especially those working in professional isolation in rural areas using digital tools and other appropriate training resources. Policy recommends development of leadership skills, strengthening human resource governance in public health system, through establishment of robust recruitment, selection, promotion and transfer postings policies.
12. Financing of Health Care:
The policy advocates allocating major proportion (upto two-thirds or more) of resources to primary care followed by secondary and tertiary care. Inclusion of cost-benefit and cost effectiveness studies consistently in programme design and evaluation would be prioritized. This would contribute significantly to increasing efficiency of public expenditure. A robust National Health Accounts System would be operationalized to improve public sector efficiency in resource allocation/ payments. The policy calls for major reforms in financing for public facilities – where operational costs would be in the form of reimbursements for care provision and on a per capita basis for primary care. Items like infrastructure development and maintenance, non-incentive cost of the human resources i.e salaries and much of administrative costs, would however continue to flow on a fixed cost basis. Considerations of equity would be factored in- with higher unit costs for more difficult and vulnerable areas or more supply side investment in infrastructure. Total allocations would be made on the basis of differential financial ability, developmental needs and high priority districts to ensure horizontal equity through targeting specific population sub groups, geographical areas, health care services and gender related issues. A higher unit cost or some form of financial incentive payable to facilities providing a measured and certified quality of care is recommended.
12.1 Purchasing of Healthcare Services: The existing Government financed health insurance schemes shall be aligned to cover selected benefit package of secondary and tertiary care services purchased from public, not for profit and private sector in the same order of preference, subject to availability of quality services on time as per defined norms. The policy recommends creating a robust independent mechanism to ensure adherence to standard treatment protocols by public and non-government hospitals. In this context the policy recognizes the need of mandatory disclosure of treatment and success rates across facilities in a transparent manner. It recommends compliance to right of patients to access information about their condition and treatment. For need based purchasing of secondary and tertiary care from non-government sector, multistakeholder institutional mechanisms would be created at Centre and State levels – in the forms of trusts or registered societies with institutional autonomy. These agencies would also be charged with ensuring that purchasing is strategic – giving preference to care from public facilities where they are in a position to do so – and developing a market base through encouraging the creation of capacity in services in areas where they are needed more. Private „not for profit‟ and „for – profit‟ hospitals would be empanelled with preference for the former, for comparable quality and standards of care. The payments will be made by the trust/society on a reimbursement basis for services provided.
13. Collaboration with Non-Government Sector/Engagement with private sector:
The policy suggests exploring collaboration for primary care services with „not- for -profit‟ organizations having a track record of public services where critical gaps exist, as a short term measure. Collaboration can also be done for certain services where team of specialized human resources and domain specific organizational experience is required. Private providers, especially those working in rural and remote areas or with under-serviced communities, could be offered encouragement through provision of appropriate skills to meet public health goals, opportunities for skill up-gradation to serve the community better, participation in disease notification and surveillance efforts, sharing and supporting certain high value services. The policy supports voluntary service in rural and under-served areas on pro-bono basis by recognised healthcare professionals under a „giving back to society‟ initiative. The policy advocates a positive and proactive engagement with the private sector for critical gap filling towards achieving National goals. One form is through engagement in public goods, where the private sector contributes to preventive or promotive services without profit- as part of CSR work or on contractual terms with the Government. The other is in areas where the private sector is encouraged to invest- which implies an adequate return on investment i.e on commercial terms which may entail contracting, strategic purchasing, etc. The policy advocates for contracting of private sector in the following activities:
13.1 Capacity building: Outsourcing of training of teachers to strengthen school health programmes by adopting neighbourhood schools for quarterly training modules.
13.2 Skill Development programmes: Recognising that there are huge gaps in technicians, nursing and para- nursing, para-medical staff and medical skills in select areas, the policy advocates coordination between National Council for Skill Development, MOHFW and State Government(s) for engaging private hospitals/private general medical practitioners in skill development.
13.3 Corporate Social Responsibility (CSR): CSR is an important area which should be leveraged for filling health infrastructure gaps in public health facilities across the country. The private sector could use the CSR platform to play an active role in the awareness generation through campaigns on occupational health, blood disorders, adolescent health, safe health practices and accident prevention, micronutrient adequacy, anti-microbial resistance, screening of children and ante-natal mothers, psychological problems linked to misuse of technology, etc. The policy recommends engagement of private sector through adoption of neighbourhood schools/ colonies/ slums/tribal areas/backward areas for healthcare awareness and services.
13.4 Mental healthcare programmes- Training community members to provide psychological support to strengthen mental health services in the country. Collaboration with Government would be an important plank to develop a sustainable network for community/locality towards mental health.
13.5 Disaster Management is another area where collaboration with private sector would enable better outcomes especially in the areas of medical relief and post trauma counselling/treatment. A pool of human resources from private sector could be generated to act as responders during disasters. The private sector could also pool their infrastructure for quick deployment during disasters and emergencies and help in creation of a unified emergency response system. Additionally sharing information on infrastructure and services deployable for disaster management would enable development of a comprehensive information system with data on availability and utilization of services, for optimum use during golden hour and other emergencies.
13.6 Strategic Purchasing as Stewardship: Directing areas for investment for the commercial health sector.
13.6.1 The health policy recognizes that there are many critical gaps in public health services which would be filled by “strategic purchasing”. Such strategic purchasing would play a stewardship role in directing private investment towards those areas and those services for which currently there are no providers or few providers. The policy advocates building synergy with “not for profit” organisations and private sector subject to availability of timely quality services as per predefined norms in the collaborating organisation for critical gap filling.
13.6.2 The main mechanisms of strategic purchasing are insurance and through trusts. Schemes like Arogyasri and RSBY have been able to increase private participation significantly. Payment is by reimbursement on a fee for service basis and many private providers have been able to benefit greatly by these schemes. The aim would be to improve health outcomes and reduce out of pocket payments while minimising moral hazards and – so that these schemes can be scaled up and made more effective. The policy provides for preferential treatment to collaborating private hospitals/institutes for CGHS empanelment and in proposed strategic purchase by Government subject to other requirements being met.
13.6.3 For achieving the objective of having fully functional primary healthcare facilities- especially in urban areas to reach under-serviced populations and on a fee basis for middle class populations, Government would collaborate with the private sector for operationalizing such health and wellness centres to provide a larger package of comprehensive primary health care across the country. Partnerships that address specific gaps in public services: These would inter alia include diagnostics services, ambulance services, safe blood services, rehabilitative services, palliative services, mental healthcare, telemedicine services, managing of rare and orphan diseases.
13.6.4 The policy advocates building synergy with “not for profit” organisations and private sector subject to availability of timely quality services as per predefined norms in the collaborating organisation for critical gaps.
13.7 Enhancing accessibility in private sector: The policy recommends a better public private healthcare interface and recognizes the need for engagement in operationalization of mechanisms for referrals from public health system. Charitable hospitals and “not for profit” hospitals may volunteer for accepting referrals from public health facilities. The private sector could also provide for increased designated free/ subsidized beds in their hospitals for the downtrodden, poor and others towards societal cause.
13.8 Role in Immunization: The policy recognizes the role of the private sector in immunization programmes and advocates their continued collaboration in rendering immunization service as per protocol.
13.9 Disease Surveillance: Towards strengthening disease surveillance, the private sector laboratories could be engaged for data pooling and sharing. All clinical establishments would be encouraged to notify diseases and provide information of public health importance.
13.10 Tissue and organ transplantations: Tissue and organ transplantations and voluntary donations are areas where private sector provides services- but it needs public interventions and support for getting organ donations. Recognising the need for awareness, the private sector and public sector could play a vital role in awareness generation.
13.11 Make in India: Towards furthering “Make in India”, the private domestic manufacturing firms/ industry could be engaged to provide customized indigenous medical devices to the health sector and in creation of forward and backward linkages for medical device production. The policy also seeks assured purchase by Government health facilities from domestic manufacturers, subject to quality standards being met.
13.12 Health Information System: The objective of an integrated health information system necessitates private sector participation in developing and linking systems into a common network/grid which can be accessed by both public and private healthcare providers. Collaboration with private sector consistent with Meta Data and Data Standards and Electronic Health Records would lead to developing a seamless health information system. The private sector could help in creation of registries of patients and in documenting diseases and health events.
13.13 Incentivising Private Sector : To encourage participation of private sector, the policy advocates incentivizing the private sector through inter alia (i) reimbursement/ fees (ii) preferential treatment to collaborating private hospitals/institutes for CGHS empanelment and in proposed strategic purchase by Government, subject to other requirements being met (iii) Non-financial incentives like recognition/ acknowledgement/ felicitation and skill upgradation to the private sector hospitals/practitioners for providing public health services and for partnering with the Government of India/State Governments in health care delivery and (iv) through preferential purchase by Government health facilities from domestic manufacturers, subject to quality standards being met.
13.14 Private sector engagement goes beyond contracting and purchasing. Private providers, especially those working in rural and remote areas, or with under-serviced communities, require access to opportunities for skill up-gradation to meet public health goals, to serve the community better, for participation in disease notification and surveillance efforts, and for sharing and support through provision of certain high value services- like laboratory support for identification of drug resistant tuberculosis or other infections, supply of some restricted medicines needed for special situations, building flexibilities into standards needed for service provision in difficult contexts and even social recognition of their work. This would greatly encourage such providers to do better. Hitherto all public training and skill provision has been only to public providers. The policy recognises the need for training and skilling of many small private providers and recommends the same.
14. Regulatory Framework:
The regulatory role of the Ministry of Health and Family Welfare- which includes regulation of clinical establishments, professional and technical education, food safety, medical technologies, medical products, clinical trials, research and implementation of other health related laws- needs urgent and concrete steps towards reform. This will entail moving towards a more effective, rational, transparent and consistent regime.
14.1 Professional Education Regulation: The policy calls for a major reform in this area. It advocates strengthening of six professional councils (Medical, Ayurveda Unani & Siddha, Homeopathy, Nursing, Dental and Pharmacy) through expanding membership of these councils between three key stakeholders – doctors, patients and society in balanced numbers. The policy supports setting up of National Allied Professional Council to regulate and streamline all allied health professionals and ensure quality standards.
14.2 Regulation of Clinical Establishments: A few States have adopted the Clinical Establishments Act 2010. Advocacy with the other States would be made for adoption of the Act. Grading of clinical establishments and active promotion and adoption of standard treatment guidelines would be one starting point. Protection of patient rights in clinical establishments (such as rights to information, access to medical records and reports, informed consent, second opinion, confidentiality and privacy) as key process standards, would be an important step. Policy recommends the setting up of a separate, empowered medical tribunal for speedy resolution to address disputes /complaints regarding standards of care, prices of services, negligence and unfair practices. Standard Regulatory framework for laboratories and imaging centers, specialized emerging services such as assisted reproductive techniques, surrogacy, stem cell banking, organ and tissue transplantation and Nano Medicine will be created as appropriate.
14.3 Food Safety: The policy recommends putting in place and strengthening necessary network of offices, laboratories, e-governance structures and human resources needed for the enforcement of Food Safety and Standards (FSS) Act, 2006.
14.4 Drug Regulation: Prices and availability of drugs are regulated by the Department of Pharmaceuticals. However, with regard to other areas of drugs and pharmaceuticals, this policy encourages the streamlining of the system of procurement of drugs; a strong and transparent drug purchase policy for bulk procurement of drugs; and facilitating spread of low cost pharmacy chain such as Jan Aushadhi stores linked with ensuring prescription of generic medicines. It further recommends education of public with regard to branded and non-branded generic drugs. The setting up of common infrastructure for development of the pharmaceutical industry will also be promoted. The policy advocates strengthening and rationalizing the drug regulatory system, promotion of research and development in the pharmaceutical sector and building synergy and evolving a convergent approach with related sectors.
14.5 Medical Devices Regulation: The policy recommends strengthening regulation of medical devices and establishing a regulatory body for medical devices to unleash innovation and the entrepreneurial spirit for manufacture of medical device in India. The policy supports harmonization of domestic regulatory standards with international standards. Building capacities in line with international practices in our regulatory personnel and institutions, would have the highest priority. Post market surveillance program for drugs, blood products and medical devices shall be strengthened to ensure high degree of reliability and to prevent adverse outcomes due to low quality and/or refurbished devices/health products.
14.6 Clinical Trial Regulation: Clinical trials are essential for new product discovery and development. With the objective of ensuring the rights, safety and well-being of clinical trial participants, while facilitating such trials as are essential, specific clause(s) be included in the Drugs and Cosmetics Act for its regulation. Transparent and objective procedures shall be specified, and functioning of ethics and review committees will be strengthened. The Global Good Clinical Practice Guidelines, which specifies standards, roles and responsibilities of sponsors, investigators and participants would be adhered to. Irrational drug combination will continue to be monitored and controlled and appropriate regulatory framework for standardization of AUSH drugs will be ensured. Clear and transparent guidelines, with independent monitoring mechanisms, are the ways forward to foster a progressive and innovative research environment, while safeguarding the rights and health of the trial participants.
14.7 Pricing- Drugs, Medical Devices and Equipment: The regulatory environment around pricing requires a balance between the patients concern for affordability and industry‟s concern for adequate returns on investment for growth and sustainability. Timely revision of National List of Essential Medicines (NLEM) along with appropriate price control mechanisms for generic drugs shall remain a key strategy for decreasing costs of care for all those patients seeking care in the private sector. An approach on the same lines but suiting specific requirements of the sectors would be considered for price control with regard to a list of essential diagnostics and equipment.
15 Vaccine Safety:
Vaccine safety and security would require effective regulation, research and development for manufacturing new vaccines in accordance with National Vaccine Policy 2011. The policy advocates commissioning more research and development for manufacturing new vaccines, including against locally prevalent diseases. It recommends building more public sector manufacturing units to generate healthy competition; uninterrupted supply of quality vaccines, developing innovative financing and creating assured supply mechanisms with built in flexibility. Units such as the integrated vaccine complex at Chengalpattu would be set up and vaccine, anti-sera manufacturing units in the public sector upgraded with increase in their installed capacity.
16 Medical Technologies:
India is known as the pharmacy of the developing world. However, its role in new drug discovery and drug innovations including bio-pharmaceuticals and bio-similars for its own health priorities is limited. This needs to be addressed in the context of progress towards universal health care. Making available good quality, free essential and generic drugs and diagnostics, at public health care facilities is the most effective way for achieving the goal. The free drugs and diagnostics basket would include all that is needed for comprehensive primary care, including care for chronic illnesses, in the assured set of services. At the tertiary care level too, at least for in-patients and out-patients in geriatric and chronic care segments, most drugs and diagnostics should be free or subsidized with fair price selling mechanisms for most and some co-payments for the “well-to-do”.
17. Public Procurement:
Quality of public procurement and logistics is a major challenge to ensuring access to free drugs and diagnostics through public facilities. An essential pre-requisite that is needed to address the challenge of providing free drugs through public sector, is a well-developed public procurement system.
18. Availability of Drugs and Medical Devices:
The policy accords special focus on production of Active Pharmaceutical Ingredient (API) which is the back-bone of the generic formulations industry. Recognizing that over 70% of the medical devices and equipments are imported in India, the policy advocates the need to incentivize local manufacturing to provide customized indigenous products for Indian population in the long run. The goal with respect to medical devices shall be to encourage domestic production in consonance with the “Make in India” national agenda. Medical technology and medical devices have a multiplier effect in the costing of healthcare delivery. The policy recognizes the need to regulate the use of medical devices so as to ensure safety and quality compliance as per the standard norms.
19. Aligning other policies for medical devices and equipment with public health goals:
For medical devices and equipment, the policy recommends and prioritises establishing sufficient labeling and packaging requirements on part of industry, adequate medical devices testing facility and effective port – clearance mechanisms for medical products.
20. Improving Public Sector Capacity for Manufacturing Essential Drugs and Vaccines:
Public sector capacity in manufacture of certain essential drugs and vaccines is also essential in the long term for the health security of the country and to address some needs which are not attractive commercial propositions. These public institutions need more investment, appropriate HR policies and governance initiatives to enable them to become comparable with their benchmarks in the developed world.
21. Anti-microbial resistance:
The problem of anti-microbial resistance calls for a rapid standardization of guidelines, regarding antibiotic use, limiting the use of antibiotics as Over-the-Counter medication, banning or restricting the use of antibiotics as growth promoters in animal livestock. Pharmaco-vigilance including prescription audit inclusive of antibiotic usage, in the hospital and community, is a must in order to enforce change in existing practices.
22. Health Technology Assessment:
Health Technology assessment is required to ensure that technology choice is participatory and is guided by considerations of scientific evidence, safety, consideration on cost effectiveness and social values. The National Health Policy commits to the development of institutional framework and capacity for Health Technology Assessment and adoption.
23. Digital Health Technology Eco – System:
Recognising the integral role of technology(eHealth, mHealth, Cloud, Internet of things, wearables, etc) in the healthcare delivery, a National Digital Health Authority (NDHA) will be set up to regulate, develop and deploy digital health across the continuum of care. The policy advocates extensive deployment of digital tools for improving the efficiency and outcome of the healthcare system. The policy aims at an integrated health information system which serves the needs of all stake-holders and improves efficiency, transparency, and citizen experience. Delivery of better health outcomes in terms of access, quality, affordability, lowering of disease burden and efficient monitoring of health entitlements to citizens, is the goal. Establishing federated national health information architecture, to roll-out and link systems across public and private health providers at State and national levels consistent with Metadata and Data Standards (MDDS) & Electronic Health Record (EHR), will be supported by this policy. The policy suggests exploring the use of “Aadhaar” (Unique ID) for identification. Creation of registries (i.e. patients, provider, service, diseases, document and event) for enhanced public health/big data analytics, creation of health information exchange platform and national health information network, use of National Optical Fibre Network, use of smartphones/tablets for capturing real time data, are key strategies of the National Health Information Architecture.
23.1 Application of Digital Health: The policy advocates scaling of various initiatives in the area of tele-consultation which will entail linking tertiary care institutions (medical colleges) to District and Sub-district hospitals which provide secondary care facilities, for the purpose of specialist consultations. The policy will promote utilization of National Knowledge Network for Tele-education, Tele-CME, Tele-consultations and access to digital library.
23.2 Leveraging Digital Tools for AYUSH: Digital tools would be used for generation and sharing of information about AYUSH services and AYUSH practitioners, for traditional community level healthcare providers and for household level preventive, promotive and curative practices.
24. Health Surveys:
The scope of health, demographic and epidemiological surveys would be extended to capture information regarding costs of care, financial protection and evidence based policy planning and reforms. The policy recommends rapid programme appraisals and periodic disease specific surveys to monitor the impact of public health and disease interventions using digital tools for epidemiological surveys.
25. Health Research:
The National Health Policy recognizes the key role that health research plays in the development of a nation‟s health. In knowledge based sector like health, where advances happen daily, it is important to increase investment in health research.
25.1 Strengthening Knowledge for Health: The policy envisages strengthening the publicly funded health research institutes under the Department of Health Research, the apex public health institutions under the Department of Health & Family Welfare, as well as those in the Government and private medical colleges. The policy supports strengthening health research in India in the following fronts- health systems and services research, medical product innovation (including point of care diagnostics and related technologies and internet of things) and fundamental research in all areas relevant to health- such as Physiology, Biochemistry, Pharmacology, Microbiology, Pathology, Molecular Sciences and Cell Sciences. Policy aims to promote innovation, discovery and translational research on drugs in AUSH and allocate adequate funds towards it. Research on social determinants of health along with neglected health issues such as disability and transgender health will be promoted. For drug and devices discovery and innovation, both from Allopathy and traditional medicines systems would be supported. Creation of a Common Sector Innovation Council for the Health Ministry that brings together various regulatory bodies for drug research, the Department of Pharmaceuticals, the Department of Biotechnology, the Department of Industrial Policy and Promotion, the Department of Science and Technology, etc. would be desirable. Innovative strategies of public financing and careful leveraging of public procurement can help generate the sort of innovations that are required for Indian public health priorities. Drug research on critical diseases such as TB, HIV/AIDS, and Malaria may be incentivized, to address them on priority. For making full use of all research capacity in the nation, grant- in- aid mechanisms which provide extramural funding to research efforts is envisaged to be scaled up.
25.2 Drug Innovation & Discovery: Government policy would be to both stimulate innovation and new drug discovery as required, to meet health needs as well as ensure that new drugs discovered and brought into the market are affordable to those who need them most. Similar policies are required for discovering more affordable, more frugal and appropriate point of care diagnostics as also robust medical equipment for use in our rural and remote areas. Public procurement policies and public investment in priority research areas with greater coordination and convergence between drug research institutions, drug manufacturers and premier medical institutions must also be aligned to drug discovery.
25.3 Development of Information Databases: There is also a need to develop information data-bases on a wide variety of areas that researchers can share. This includes ensuring that all unit data of major publicly funded surveys related to health, are available in public domain in a research friendly format.
25.4 Research Collaboration: The policy on international health and health diplomacy should leverage India‟s strength in cost effective innovations in the areas of pharmaceuticals, medical devices, health care delivery and information technology. Additionally leveraging international cooperation, especially involving nations of the Global South, to build domestic institutional capacity in green-field innovation and for knowledge and skill generation could be explored.
26. Governance
26.1 Role of Centre & State: One of the most important strengths and at the same time challenges of governance in health is the distribution of responsibility and accountability between the Centre and the States. The policy recommends equity sensitive resource allocation, strengthening institutional mechanisms for consultative decision-making and coordinated implementation, as the way forward. Besides, better management of fiduciary risks, provision of capacity building, technical assistance to States to develop State-specific strategic plans, through the active involvement of local self-government and through community based monitoring of health outputs is also recommended. The policy suggests State Directorates to be strengthened by HR policies, central to which is the issue that those from a public health management cadre must hold senior positions in public health.
26.2 Role of Panchayati Raj Institutions: Panchayati Raj Institutions would be strengthened to play an enhanced role at different levels for health governance, including the social determinants of health. There is need to make Community Based Monitoring and Planning (CBMP) mandatory, so as to place people at the centre of the health system and development process for effective monitoring of quality of services and for better accountability in management and delivery of health care services.
26.3 Improving Accountability: The policy would be to increase both horizontal and vertical accountability of the health system by providing a greater role and participation of local bodies and encouraging community monitoring, programme evaluations along with ensuring grievance redressal systems.
27. Legal Framework for Health Care and Health Pathway
One of the fundamental policy questions being raised in recent years is whether to pass a health rights bill making health a fundamental right- in the way that was done for education. The policy question is whether we have reached the level of economic and health systems development so as to make this a justiciable right- implying that its denial is an offense. Questions that need to be addressed are manifold, namely, (a) whether when health care is a State subject, is it desirable or useful to make a Central law, (b) whether such a law should mainly focus on the enforcement of public health standards on water, sanitation, food safety, air pollution etc, or whether it should focus on health rights- access to health care and quality of health care – i.e whether focus should be on what the State enforces on citizens or on what the citizen demands of the State? Right to healthcare covers a wide canvas, encompassing issues of preventive, curative, rehabilitative and palliative healthcare across rural and urban areas, infrastructure availability, health human resource availability, as also issues extending beyond health sector into the domain of poverty, equity, literacy, sanitation, nutrition, drinking water availability, etc. Excellent health care system needs to be in place to ensure effective implementation of the health rights at the grassroots level. Right to health cannot be perceived unless the basic health infrastructure like doctor-patient ratio, patient-bed ratio, nurses-patient ratio, etc are near or above threshold levels and uniformly spread-out across the geographical frontiers of the country. Further, the procedural guidelines, common regulatory platform for public and private sector, standard treatment protocols, etc need to be put in place. Accordingly, the management, administrative and overall governance structure in the health system needs to be overhauled. Additionally, the responsibilities and liabilities of the providers, insurers, clients, regulators and Government in administering the right to health need to be clearly spelt out. The policy while supporting the need for moving in the direction of a rights based approach to healthcare is conscious of the fact that threshold levels of finances and infrastructure is a precondition for an enabling environment, to ensure that the poorest of the poor stand to gain the maximum and are not embroiled in legalities. The policy therefore advocates a progressively incremental assurance based approach, with assured funding to create an enabling environment for realizing health care as a right in the future.
28. Implementation Framework and Way Forward
A policy is only as good as its implementation. The National Health Policy envisages that an implementation framework be put in place to deliver on these policy commitments. Such an implementation framework would provide a roadmap with clear deliverables and milestones to achieve the goals of the policy.
Sign up for our newsletter and special offers
By subscribing you agree to receive our newsletter and related offers
Dun & Bradstreet, headquartered in Jacksonville, Florida, offers information on commercial credit as well as reports on businesses. Most notably, it is recognizable for its Data Universal Numbering System (DUNS numbers); these generate business information reports for companies around the globe. Click here to view listing.

Bisnode is a company that offers decision support in the form of digital business, marketing and credit information. Founded in 1989, Bisnode is now a Dun & Bradstreet company. Bisnode is present in 19 European countries and has its headquarters in Stockholm, Sweden. Click here to view listing.
Disclaimer: Content of this website is for information purposes only. Some of the images/videos could be solely for representation purposes. Please note the date of last review or update on all articles and other content. No content on this site or on any of HealthySpan’s social media handles, regardless of date, including but not limited to, live fitness sessions etc., should ever be used as a substitute for direct medical advice from your doctor, other qualified clinician or a certified fitness trainer. HealthySpan Wellness does not claim to treat any disease nor does it claim that any organic nutrition or any other aspects narrated can do so. Appropriate lifestyle habit modifications are not a substitute for medical treatment. However, HealthySpan Wellness believes lifestyle disorders viz. obesity or other obesity-related disorders can be effectively managed by positive changes to lifestyle habits, viz., diet, nutrition, exercise, sleep, developing a positive mental attitude. No one can guarantee different individuals will have same results. Individual experiences with the wellness programs may vary. Please read ‘Terms and conditions of use’ and ‘Privacy policy’ for further information.